Today
16th October 2017 marks the Centenary of my father qualifying as a doctor.
The occasion is recorded in my grandmother’s diary, and I have his old certificates, though some certificates have later dates.
The occasion is recorded in my grandmother’s diary, and I have his old certificates, though some certificates have later dates.
It
thus seems like an appropriate day to publish some of his obervations about
what life was like while training to be a doctor (he wrote about this in the
1960s when he retired)
When the First War broke out I joined the Officer Training Corps (OTC) instead of starting Hospital work in August and completed the three months basic training in November.
Arthur in OTC uniform 1914
However
it was then discovered that the war looked like being a long one, and those
undergraduates who were medical students with only their Finals to do were to
continue hospital work until qualified and then go into the RAMC as Medical
Officers.
Because
I was one of those to whom this applied I started clinical work as an
out-patient dresser at the General Hospital Bristol in November and attended
normal lectures in Medicine, Surgery, and Pathology at the University Medical
School.
The
work before me meant a whole three years work before I could complete my quota
and take the final exam.
Christmas 1914
Depleted
staff, extra work for everyone, no students junior to me following me gave me
and my generation a great deal more responsibility and experience than would
have occurred in normal times. Although the standard set for the conjoint
diplomas of MRCS and LRCP were the same as the London MB degree, the exams
could be taken in parts, 1. Medicine, 2. Surgery, 3. Midwifery, whereas for the
degree the whole had to be taken at once in an exam lasting nearly three weeks.
So
I, and most of the others took this chance, thinking that if we survived the
war, if we had once got qualified and into the RAMC we could return to hospital
and take the degree afterwards.
The
house surgeons etc. were so reduced in numbers that final year students acted
as such, so that one could be an obstetric house surgeon under a qualified
“chief” for some months before taking the midwifery exam, and so be able to
concentrate on the subject. Then act as house physician before the medicine
exam, and as house surgeon before the surgery. In this way one could and did
enhance one’s chance of success.
The
first year’s study entails the same course as that for the Science B.Sc. degree
so that the medical students are a minority group among the science ones. The
latter take mathematics and the medicals Zoology, which consists of the study
and dissection of the earthworm, dogfish, frog and rabbit - a preliminary to
the larger study of human anatomy. Physiology and Human anatomy take up the two
following years and are carried out in the medical school proper.
Daily
lectures, laboratory work most mornings in physiology and dissection in the
anatomy department were the order of the day.
Anatomy
lectures were made most interesting by the superb drawings in coloured chalks
on the blackboard by the Professor - Edward Fawcett - then coming towards the
end of his long career as anatomist and embryologist.
Professor
Stanley Kent and Rendle Short were the leading teachers in Physiology. I had
coaching from the latter prior to taking the London Exam. He was already the
author of more than one book, and later devoted his attention to surgery and
became professor of that subject at the University. He was a most brilliant
teacher and was a member of the Plymouth Brethren and prayed before each
operation. He and Leonard* had been fellow students and between them they shared a very great number of
medals and prizes.
*Leonard was my father's half brother who was ten years older than him and qualified as a doctor ten years earlier. Leoard too joined the RAMC as an army doctor, but was gassed in 1917; he survived and while recovering took the exams to qualify as a surgeon.
A
queer character I met in these years was the late Oliver Charles Minty Davies
(Known always as OCM) he was then a lecturer in Chemistry but was studying for
a medical degree as well. Tall, thin and mysterious he was exactly like
Sherlock Holmes in appearance. He qualified in medicine and obtained a Bristol
M.D. gave up chemistry and became Consultant Physician to the Bristol
Children’s Hospital and after a few years studied Law and became a barrister.
The last time I saw him he was bewigged and appearing as a counsel at the
Assize Court in Taunton where I was appearing as a witness.
Having
passed my second MB exam at the outbreak of the 1914-18 war I spent three years
from Christmas 1914 until I qualified in October 1917 in and out of the Bristol
General Hospital (The BGH).
During
this period all the honorary staff were in Khaki as territorial RAMC officers
(either Majors or Colonels) all attached to the 2nd Southern General
Military Hospital with main buildings at the Southmead County Council Hospital
and branches at the BGH and the Bristol Royal Infirmary. As all young qualified
men, if fit, were in the RAMC the house staff was very deficient in numbers or
else consisted of men unfit for military service. All through my time there we
had George Cromie a middle-aged New Zealander (with a gastric ulcer which gave
him frequent haemorrhages) and the two brothers Lim who were Chinese. An
occasional woman arrived for six months and all the students as they qualified
were automatically called up, but equally automatically served three months as
residents before actually going into uniform and departing. These men covered
the senior students usually in the final year who were acting house surgeons
and physicians. One “lived-in” while doing surgical dressers jobs, also as
midwifery students or as resident house men, and I spent my time during the
three years half “in” and half “out” living at home.
Lectures
had to be attended daily at the medical school at 9am and 5pm and the rest of
the day we were at the Hospital.
It
seems incredible in the nineteen sixties to think of our limitations in those
days. Iodine, lypsol, potassium permanganate, and acetic acid were our
“antiseptics” to begin with although early in 1915 Eusol appeared and was
fairly quickly followed by flavine and acriflavin as less irritating and more
efficient antiseptics.
Antibiotics,
“sulpha” drugs, cortisones etc were unheard and undreamt of. During my time in
hospital I never saw a blood transfusion given; anaesthetics (chloroform and
ether) were given from a drop bottle onto a mask; and hypodermic injections
were uncommon things and usually given by a “sister” - I hardly ever gave one
and yet an amputation of a finger or the circumcision of an infant were things
I did regularly on Tuesdays and Thursdays from my very first week in “Casualty”
department when I arrived there at the end of 1914.
My father amputating a thumb!
(The photo had to be staged to a certain extent to make it
possible to take a photo at all given the light levels indoors)
All
traumatic wounds with broken skin went septic as a matter of course and were
treated with hot foments of the above mentioned lotions or perhaps the
foul-smelling iodoform powder which “disguised” the smell of the suppurating
wounds.
Operations
in the theatre did remain clean afterwards - the skin being scrubbed and then
painted with iodine, picric acid, or lolio carbolic first according to the
fancy of each particular surgeon. Sterile gowns and gloves were worn together
with caps and masks in the theatre, but staff and spectators came into the
theatre in their ordinary clothes and muddy boots under their gowns!
I
did my surgical dressing for Mr C.A. Moore, a very good teacher indeed, but a
quick-tempered man who let his nurses and students know when he was displeased
in no uncertain manner. He was a quick and neat operator, but like all the
surgeons of that time he never completely closed an operation incision but
always put in a rubber drainage-tube for a few days. His quick-temper like that
of several surgeons reminds me of the saying “Physicians are gentlemen and
surgeons are surgeons.” I never experienced any bad temper or impatience in any
of the physicians I made contact with.
The
one for whom I did my clinical clerking was John Michell Clarke who was
professor of Medicine in the University. A brilliant diagnostician and almost
uncanny in the accuracy of his prognosis he was the most thorough doctor I have
ever met - and he taught thoroughness and attention to detail to all his
students.
The
clinical clerk who was of course junior to the other students who came with the
professor on his teaching rounds had to carry a book the size of a large ledger
in which all the students’ clinical notes had been set down. At each bedside he
had to read out these notes for all to hear accompanied by a running commentary
on them by the professor. One was always told what had been missed, left out,
or done the wrong way; but always politely and
always given a word of praise and congratulation for good notes.
Michell
Clarke was afflicted with a slight impediment in his speech which made him
sound slightly stupid, but anyone less stupid it would be hard to find. He
always knew the family history of all his patients from the clerk’s notes and
he always remembered them when the patient left the hospital. Frequently he
would go up to the patient who was leaving and say “Ah, my man, you will be
going home tomorrow, here’s twopence for your tram.” It was not until many
years afterwards that I was talking to the then sister of his ward and she told
me that there was a gold sovereign between the two pennies. I wonder if that
kind of practical and generous treatment goes on nowadays - I very much doubt
it.
“Living
in” hospital work had in wartime a great advantage that food was much more
plentiful than it was at home and apart from inadequate sugar to which one
added saccharin and margarine in place of butter, there was no actual shortage
of food. Of course by the last year of the war when rationing was really rigid
I had left and was in the RAMC abroad.
Midwifery
was the thing I think I enjoyed most even though I was scared stiff to begin
with. As only abnormal cases were admitted to hospital nearly all of it was
done by the students outside “on the district” - otherwise in the slums and
working class district round the hospital. The student and the midwifery sister
had to walk to (and find) the house, and as far as the student was concerned he
had never seen the patient before, and no ante-natal examinations had been
carried out. Thirty cases had to be attended before one could sit for the
midwifery exam, but as I was keen and lucky enough to act as a combined student
and obstetric house surgeon, and spend five months on the job instead of three,
I managed to do seventy cases - nearly all of them outside “on the district”. I
am afraid by modern standards it does not appear as good as it did to us then -
no anaesthetics, suturing only for grossly ruptured perineum, but fantastic
patience and attention given by the sisters to the mothers and infants.
Conditions were frequently appalling - dirt, darkness, drinking by the
relatives, and livestock in abundance. On our return to hospital the bathroom
and a cake of soap was the first thing necessary - one sister had a record
“catch” in my time of 14 bugs and 78 fleas! I never reached anything like that
total.
My
last nine months at the BGH I spent as Casualty Officer - six months while
unqualified and three months qualified. During the last three months I also
managed to have riding lessons in preparation for the RAMC in which all medical
officers had to be able to ride.
I
had always intended to do general practice after qualifying and leaving the
RAMC, and this I did, but I never dreamed that nine years after leaving when I
was living and practising in Bridgwater I should return to the BGH as a
clinical assistant in gynaecology to Professor Drew-Smythe, and hold an
Out-patient clinic once a week for twelve years. An honorary post, but one
which gave me most valuable experience and friendly contacts. During this time
Drew-Smythe and I started ante-natal examinations of abnormal and then normal
cases sent up to the clinic by outside practitioners - quite a new departure;
and I also introduced Dettol to Drew-Smythe as a vast improvement on Lysol as
an antiseptic lotion in midwifery.
When
I first entered the RAMC I first did a short course in venereal disease** at
Rochester Row Military Hospital in London, during which time I stayed in a
hotel - experienced an Zeppelin raid doing damage unpleasantly close to me one
night whilst there.
**My father often recounted the story of giving injections at said time. Row upon row of
bare bottomed soldiers lined up bent forward for him and a sister with a
trolley to walk along. The trolley providing a fresh syringe for each new pair
of buttocks till things reached the point where he risked something akin to
Repetitive Strain Injury, or going permanently cross-eyed. I believe a top VD
job was offered to him after the war, but in the light of this one can
understand perhaps why it was turned down.
At
the hospital all the specialists and consultants (honorary of course in those
days) always wore top hats and frock or morning coats - although if raining a
bowler might be a substitute. During my stay in Hospital during the war they
many of them gave up their horses and carriages and appeared in motorcars
driven by chauffeurs, but many more often used the tramcars.
I
like the rest of the medical students walked to and from the hospital, although
one or two used bicycles and by 1917 there were one or two with motorbikes. And
a rush it was sometimes to get between University for lectures and the Hospital
for clinical work.
In 1974 my father wrote some more about his time at Medical School.
Sixty five years ago last
month I started as a medical student at Bristol University University
College University of Bristol Medical School
For a University the grey
stone buildings surrounding three sides of a courtyard facing the playing
fields of Bristol
Grammar School
During my first
year building was going on continuing the Arts and Science Faculty through to
Woodland Road so that there then became two fronts - one to Woodland Road and
one to University Road. Later on during my time a further enlargement was made
by taking over the old Bristol Blind Asylum facing the top of Park Street
Since the Second World War Woodland Road
During my first year the
Chemistry and Biology departments were gloomy, old fashioned and most
inconvenient, and entailed going up and down long narrow corridors and
staircases.
Most of the old college
staff carried on although professor Conway Morgan ceased to be Principal and
was replaced by Sir Isambard Owen as vice-chancellor. Professor Fawcett was
head of the Faculty of Medicine and in charge of the Anatomy department;
Francis Frances was professor of Chemistry and Priestly head of Biology jointly
with Professor Reynolds. Physics was professor Shattock with AM Tyndall one of
his staff and subsequent successor.
Contemporary undergraduates
of mine in the Medical
School Bristol
Hospitals Africa , and Douthwaite, who became a senior physician at
Guy’s Hospital.
The 1914-18 War caused a
great scattering, but after that was over many of us practised in Somerset
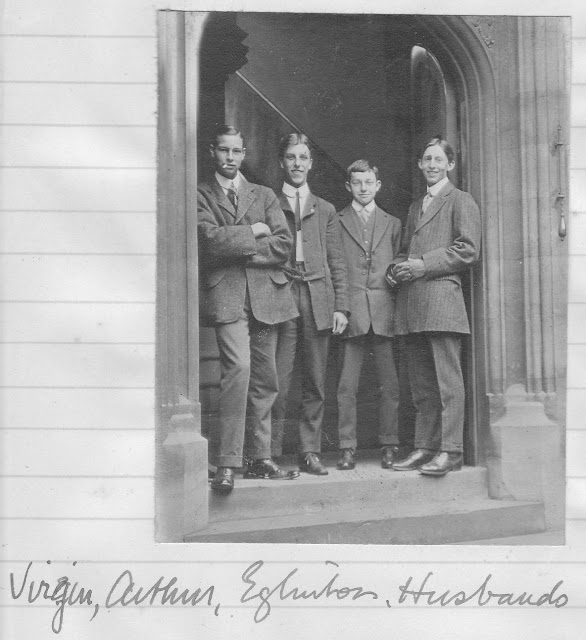
My father is second from the left, Eglington, who he mentions, is the second from the right
My father is seated on the right with his legs crossed. He did not label this photo but given the names he mentuons in his account I expect they include the following: Tasker, James Drew-Smythe#, Wilfred Adams, Clement Chesterman##, Douthwaite, Burns, Husbands, Archer, Eglinton and Norman Cooper.
(##For more info about James Drew-Smythe see here)
##For more info about Sir Clement Chesterman see his obituary here
(##For more info about James Drew-Smythe see here)
##For more info about Sir Clement Chesterman see his obituary here
My grandfather took this photograph of my father around the time he qualified, (and made him go onto the roof so there was enough natural light for a short exposure time)
1918 and my father is a Doctor in the RAMC







Geen opmerkingen:
Een reactie posten